Abstract
Background
Multiple myeloma (MM) is associated with a 9-fold increased risk of venous thromboembolism (VTE). Current guidelines support routine thromboprophylaxis in select patients (ASCO, IMWG). The 2015 ASCO guidelines recommend low-molecular-weight heparin or low-dose aspirin in patients receiving immunomodulatory drugs (IMIDs) in combination with chemotherapy and/or dexamethasone. The IMWG guidelines recommend low-dose aspirin for MM patients with one or no VTE risk factors including those on lenalidomide in combination with low-dose dexamethasone, melphalan, or doxorubicin. Two randomized trials support thromboprophylaxis in patients receiving lenalidomide and thalidomide; however, patients with a prior history of VTE were excluded from participation (Palumbo 2011, Larocca 2012). We assessed the association between aspirin use and VTE in a large cohort of patients with MM.
Methods
Patients diagnosed with MM within the Veterans Health Administration between September 1, 1999 and December 31, 2013 were identified in the Veterans Administration Central Cancer Registry (VACCR) using International Classification of Diseases (ICD)-O3 codes 9732/3. We retrospectively followed the cohort through December 2014. We excluded patients who did not receive MM-directed therapy within 6-months of diagnosis. We collected baseline information on demographics, comorbidities, laboratory data, MM-directed therapy, and use of aspirin, warfarin, and statins. All drug therapy was analyzed as time-varying. Using a previously validated algorithm, (Sanfilippo, 2015), we identified patients diagnosed with VTE after MM diagnosis by a combination of ICD-9 code for VTE plus pharmacologic treatment for VTE or IVC filter placement. We used competing risk analysis to assess the association between aspirin use and incident VTE while adjusting for known VTE risk factors and for death as a competing event.
Results
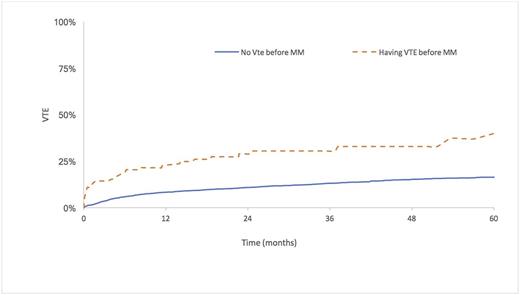
We identified a cohort of 4,892 patients of whom 586 developed VTE. A total of 1,888 patients received aspirin therapy after MM diagnosis while 862 received warfarin therapy. After adjusting for known potential VTE risk factors, including history of VTE and use of IMIDs, aspirin was not associated with a decreased risk of VTE (adjusted Hazard Ratio (aHR) 1.18; 95% Confidence Interval (CI) 0.92-1.52). Warfarin use was associated with a trend towards reduction in risk of VTE (aHR 0.77; 95% CI 0.53-1.12). Risk factors for VTE after MM diagnosis included: history of prior VTE (aHR 3.83; 95% CI: 2.68-5.48), lenalidomide (aHR 2.36; 95% CI 1.82-3.05), and thalidomide (aHR 2.60; 95% CI: 2.09-3.24). The figure shows the high probability of developing VTE after MM diagnosis, especially among patients with a history of VTE.
Conclusions
Lenalidomide, thalidomide, and a prior VTE increased the risk of VTE after MM diagnosis. Patients with such history should be considered high risk for VTE. In this high-risk population, aspirin may not provide adequate thromboprophylaxis.
Sanfilippo: Bristol Myers Squibb: Speakers Bureau. Carson: Seattle Genetics: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.